PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 36(3); 2019 > Article
-
Original article
Determining the correlation between outdoor heatstroke incidence and climate elements in Daegu metropolitan city -
Jung Ho Kim1
 , Hyun Wook Ryoo2
, Hyun Wook Ryoo2 , Sungbae Moon2
, Sungbae Moon2 , Tae Chang Jang3
, Tae Chang Jang3 , Sang Chan Jin4
, Sang Chan Jin4 , You Ho Mun1
, You Ho Mun1 , Byung Soo Do1, Sam Beom Lee1
, Byung Soo Do1, Sam Beom Lee1 , Jong-yeon Kim5
, Jong-yeon Kim5
-
Yeungnam University Journal of Medicine 2019;36(3):241-248.
DOI: https://doi.org/10.12701/yujm.2019.00248
Published online: July 2, 2019
1Department of Emergency Medicine, Yeungnam University College of Medicine, Daegu, Korea
2Department of Emergency Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
3Department of Emergency Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea
4Department of Emergency Medicine, Keimyung University School of Medicine, Daegu, Korea
5Department of Preventive Medicine, Catholic University of Daegu School of Medicine, Daegu, Korea
- Corresponding author: Jong-yeon Kim, Department of Preventive Medicine, Catholic University of Daegu School of Medicine, 33, Dooryugongwon-ro 17-gil, Nam-gu, Daegu 42472, Korea Tel: +82-53-650-4494, Fax: +82-53-2675-4752, E-mail: kom824@cu.ac.kr
Copyright © 2019 Yeungnam University College of Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 6,372 Views
- 79 Download
- 1 Crossref
Abstract
-
Background
- Heatstroke is one of the most serious heat-related illnesses. However, establishing public policies to prevent heatstroke remains a challenge. This study aimed to investigate the most relevant climate elements and their warning criteria to prevent outdoor heatstroke (OHS).
-
Methods
- We investigated heatstroke patients from five major hospitals in Daegu metropolitan city, Korea, from June 1 to August 31, 2011 to 2016. We also collected the corresponding regional climate data from Korea Meteorological Administration. We analyzed the relationship between the climate elements and OHS occurrence by logistic regression.
-
Results
- Of 70 patients who had heatstroke, 45 (64.3%) experienced it while outdoors. Considering all climate elements, only mean heat index (MHI) was related with OHS occurrence (p=0.019). Therefore, the higher the MHI, the higher the risk for OHS (adjusted odds ratio, 1.824; 95% confidence interval, 1.102–3.017). The most suitable cutoff point for MHI by Youden’s index was 30.0°C (sensitivity, 77.4%; specificity, 73.7%).
-
Conclusion
- Among the climate elements, MHI was significantly associated with OHS occurrence. The optimal MHI cutoff point for OHS prevention was 30.0°C.
- Increasing greenhouse gas emissions and consequent global warming continue to be major environmental issues. The average global temperature in July 2016 was 0.82°C higher than the mean temperatures from 1951 to 1980 [1]. Global warming may cause previously unobserved weather patterns, including extreme heat and cold. Prolonged exposure to high temperatures can cause various heat-related illnesses, such as edema, cramps, syncope, exhaustion, and heatstroke, which can lead to death in severe cases [1-6]. For example, heatwaves, excessively hot weather lasting for days or weeks, claimed 14,800 lives in France in 2003 and 55,000 lives in Russia in 2010. In 2009, Australia reported a 14-fold increase in hospitalizations due to heat-related illnesses [2,5,6]. In Korea, heatwaves caused 442 heat-related deaths from 1991 to 2011; in Seoul, over 80 excess deaths occurred during the day in 1994 [7,8].
- One of the most serious heat-related illnesses is heatstroke. It is typically characterized by a core body temperature exceeding 40℃ and central nervous system (CNS) abnormalities, such as altered mental status or seizure [2-6,9]. Older people, people with dehydration, individuals diagnosed with alcoholism, and individuals with previous neuropsychiatric disorders are more susceptible to heatstroke [6,9,10]. A heatwave that affected Pakistan during Ramadan in 2015 caused heatstroke in 78 patients within a period of 3 days; unfortunately, 42 of these patients died [11]. Several countries have implemented heat-health alert systems to prevent the occurrence of such heat-related health conditions. However, the specific methods and warning criteria for these systems vary by country [12-16]. The Korea Meteorological Administration (KMA) is currently operating a heat alert system based on maximum daily temperatures [17-19]. Based on this alert system, the number of summer heatwaves (maximal daily temperature over 33°C) in Daegu, one of the hottest regions in Korea, have increased from 25 days in 2011 to 32 days in 2016 and 51 days in 2013 [17]. However, this system does not consider the heat index, which is a measure of the actual heat-related stress in the human body.
- Although there have been numerous studies regarding heatstroke, most of them have focused on its pathophysiology or complications. Only a few studies have examined the correlations between heatstroke and various climate elements. Previous studies aimed at identifying the most predictive climate elements and warning criteria for preventing heatstroke are limited. Therefore, we aimed to examine the correlations between outdoor heatstroke (OHS) incidence and climate elements in a single metropolitan city in Korea in order to determine the most relevant climate elements and their warning criteria to prevent heatstroke.
Introduction
- 1. Study participants
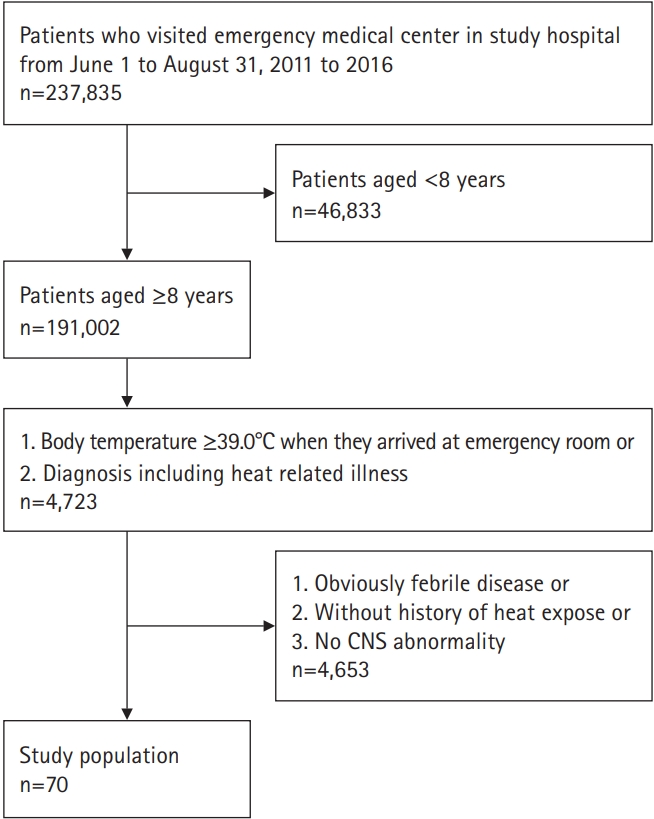
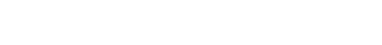
- To compare the differences in the climate elements between the days when the heatstroke occurred and days that heatstroke did not occur, we considered all days during the summer (June 1 to August 31) of 2011 to 2016. To identify all heatstroke cases in the Daegu metropolitan city in those periods, we reviewed the medical records of 237,835 patients who were admitted to the emergency room (ER) during those periods in one regional emergency medical center and four local emergency medical centers.
- The diagnosis of heatstroke was based on a patient’s medical history and clinical features after ruling out other febrile diseases. In order to determine the appropriate study participants, the following inclusion criteria were used. An age limit of ≥8 years was applied to ensure diagnostic accuracy, as the clinical presentation of heatstroke is similar to that of septicemia in children aged <8 years [3]. With regard to the inclusion criteria, using the final diagnosis is simple but it is likely that the diagnostic input may be missing; hence, we used the following two criteria: (1) having an initial body temperature of ≥39°C upon admission and (2) classified using diagnosis codes that indicate heat-related illnesses. A body temperature limit of ≥39°C upon admission was used to minimize missing cases, as the body temperature of patients could have been measured as <40°C when they arrived at the ER [10,20,21]. A total of 4,723 patients aged ≥8 years who met one of these criteria were initially selected. Subsequently, individuals (1) with obviously febrile disease, (2) without history of heat exposure, and (3) with no CNS abnormalities were excluded; after excluding these patients, 70 were ultimately classified as heatstroke patients [2,5,6] (Fig. 1). To analyze the relationship between heatstroke incidence and climate elements, we only included OHS patients (excluding indoor heatstroke [IHS] patients) and those who developed heatstroke in unknown locations.
- 2. Data collection
- We retrospectively reviewed the medical records of patients admitted to each emergency medical center. With regard to the general characteristics, age, sex, location, circumstances when heatstroke occurred, and arrival type and time were considered. With regard to the clinical characteristics, onset time, body temperature upon arrival, state of consciousness upon arrival, systolic blood pressure upon arrival, underlying diseases, intubation, and treatment outcome were considered. If the onset time was unknown, the time when the individual was last observed as normal was determined. With regard to the outcome, individuals whose records confirmed a discharge following clinical recovery (i.e., normal consciousness level and body temperature) were classified as having good outcomes. Patients whose records indicated fatality or who were transferred to another medical center, as they had no signs of clinical recovery, were classified as having poor outcomes.
- The following climate elements for the corresponding time period were obtained from the KMA website: the minimum temperature, maximum temperature, mean temperature, mean relative humidity, mean wind speed, mean daylight hours, heatwave, and daily mean heat index (MHI) in the Daegu area. The daily MHIs obtained were classified as follows: very low (<27°C), low (27–31°C), ordinary (32–40°C), high (41–53°C), very high (54–65°C), and dangerous (≥66°C) according to the standards currently used by the KMA. Data collection of this retrospective study was commenced after approval by the Yeungnam University Hospital Institutional Review Board (IRB No. 2017-03-023).
- 3. Statistical analysis
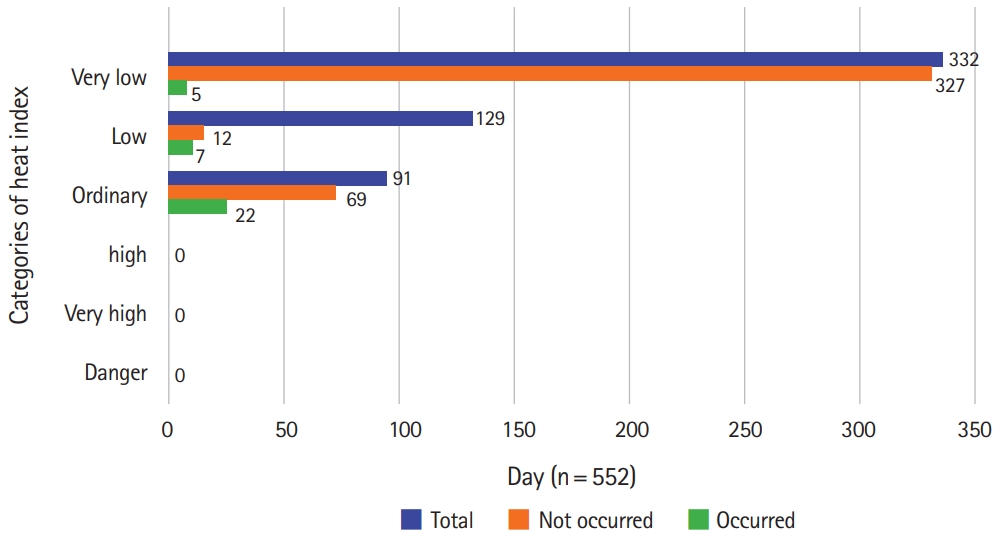
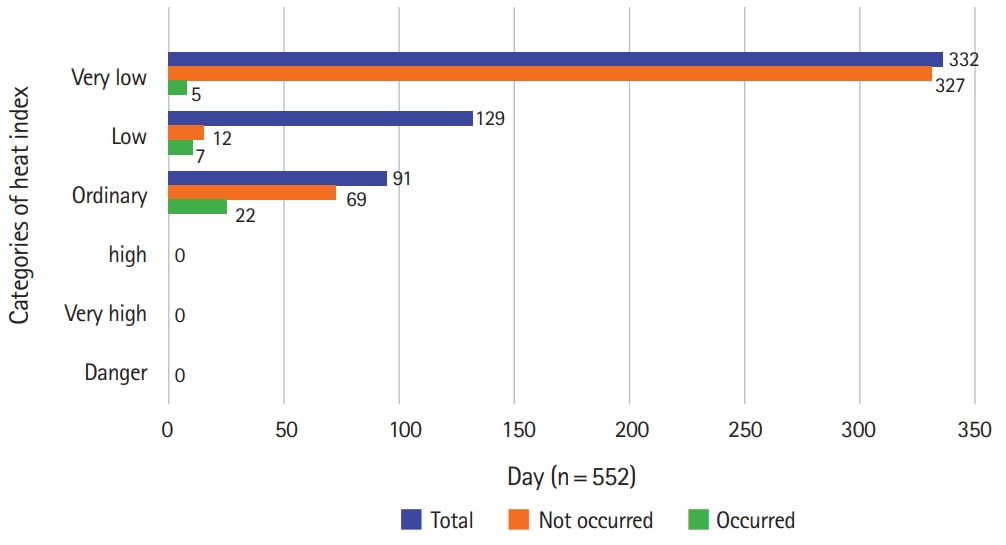
- The distributions of MHIs and OHS incidence by stage are presented (Fig. 2). To identify the individual effects of daily climate elements on OHS occurrence, a logistic regression analysis was performed with each climate element as an independent variable and OHS occurrence as the dependent variable. Simultaneously, to identify the element that was closely correlated with OHS occurrence, a logistic regression analysis was performed using all elements as independent variables, except the days when IHS occurred. To determine the appropriate cutoff point for the most correlated climate element to prevent OHS, the sensitivity, specificity, and Youden’s index (sensitivity+specificity–1) were calculated.
- All statistical analyses were performed using IBM SPSS version 21.0 (IBM Co., Armonk, NY, USA), with the significance level set at p<0.05.
Materials and methods
- Of the total 70 heatstroke patients, 45 were OHS patients, 17 were IHS patients, and 8 had heatstroke in an unknown location. The baseline characteristics of heatstroke patients are described in Table 1.
- There were no significant differences in the climate elements between IHS and OHS patients. Furthermore, MHI levels between the two groups were also found to be insignificant. All patients developed heatstroke at an MHI level below “ordinary” (Table 2).
- During the study period (552 days), the day of heatstroke occurred was 47 days, including the 34 days in which OHS occurred. The MHI of the 34 days in which OHS occurred were higher than that of the other 518 days (32.1±4.5°C and 26.1±4.2°C, respectively). A 1°C increase in the MHI was significantly associated with a 1.393-fold increase in the risk for OHS (95% confidence interval [CI], 1.255–1.546). The mean, maximum, and minimum daily temperatures and diurnal temperature range of OHS occurred days were also greater than those of the other days. A 1°C increase in the mean, maximum, and minimum daily temperatures and diurnal temperature range was significantly associated with a 1.710-fold (95% CI, 1.436–2.036), 1.787-fold (95% CI, 1.489–2.145), 1.450-fold (95% CI, 1.246–1.688), and 1.352-fold (95% CI, 1.175–1.557) increase in the risk for OHS, respectively. Similarly, a 1-hr increase in daylight hours was significantly associated with a 1.397-fold increase risk for OHS (95% CI, 1.227–1.589).
- A 1% increase in mean humidity was significantly associated with a 0.938-fold reduction in the risk for OHS (95% CI, 0.909–0.969). A 1 m/sec increase in the mean wind speed was also significantly associated with a 0.371-fold reduction in the risk of OHS (95% CI, 0.199–0.694). However, when all climate elements were considered simultaneously, only the daily MHI was found to significantly increase OHS risk: a 1°C increase in the daily MHI resulted in a 1.824-fold (95% CI, 1.102–3.017) increase in OHS risk (Table 3).
- The sensitivity, specificity, and Youden’s index, with exception of the days when heatstroke occurred indoors, were calculated to determine the warning criteria for OHS. The most suitable cutoff point was confirmed to be a daily MHI of 30.0°C (Youden’s index, 0.511; sensitivity, 77.4%; specificity, 73.7%; Table 4).
Results
- Extreme weather phenomena due to global warming continue to occur worldwide, with a significant impact on human life [22-26]. Heatwaves are one of the most concerning meteorological conditions expected to cause damage as climate change progresses [7,27-29]. An individual affected by heatstroke loses the ability to regulate body temperature due to damage to the hypothalamic thermoregulatory system following prolonged exposure to high temperatures [30,31]. A sustained elevated core temperature can damage a number of internal organs, which can lead to a life-threatening situation [2-4,21]. Thus, many countries have been making efforts to reduce the disease burden associated with heat-related illnesses, including the implementation of effective heat alert systems [15,16,32-37]. An effective alert system requires the selection of the most appropriate climate elements and their warning criteria to predict heatstroke occurrence [38].
- In the literature, there are conflicting findings regarding which elements are most predictive of heatstroke occurrence. Some studies have reported that heat index is strongly correlated with the number of patients admitted to the ER due to heat-related illnesses, which suggests the application of the heat index as a predictor of heat-related illness [19,39,40]. Other studies have reported that the daily maximum temperature is a more appropriate predictor of heatstroke occurrence than the heat index [8,28,41]. Heat index is the biometeorological indicator used by the United States National Weather Service [19]. It is calculated by measuring the dry-bulb Fahrenheit temperature and relative humidity to estimate the heat burden according to outdoor conditions.
- Based on our study, various climate elements, including the mean, maximum, and minimum daily temperatures; diurnal temperature variations; daylight hours; and the MHI, were significant risk factors for OHS occurrence, whereas mean humidity and mean wind speed were significant protective factors. This finding is congruent to the fact that, aside from prolonged exposure to high heat, dry conditions and poor ventilation increase the risk of heatstroke. However, after simultaneously considering these climate elements, we found that the MHI was the only effective predictor of OHS incidence. The risk of OHS increased significantly by 1.82-fold for each 1°C increase in the MHI. The finding that the MHI was the only significant predictor of OHS may be attributed to the fact that the MHI is a biometeorological index that incorporates both dry bulb temperature and relative humidity for measuring climate-related heat stress in the human body. Thus, the heat index, which reflects both air temperature and humidity, may be more useful for predicting OHS incidence than the maximum daily temperature, which only reflects air temperature.
- In South Korea, the KMA has been operating heatwave alerts system based on the maximum daily temperature. Additionally, the KMA also provides daily heat index values, using the heat index categories of low (27–31°C), ordinary (32–40°C), high (41–53°C), very high (54–65°C), and dangerous (≥66°C) based on the heat index classifications from the National Oceanic and Atmospheric Administration [17]. However, these categories are not actively used as an alert index as there is no scientific evidence indicating the most appropriate cutoff point to predict heatstroke occurrence [42].
- During the study period (552 days), 332 days were categorized as very low risk, 129 days as low risk, and 91 days as ordinary risk, based on the heat index category. Significantly, none of the days were categorized as high, very high, or dangerous. Of the 34 days in which heatstroke occurred, 22 days were categorized as ordinary risk, 12 days as low risk, and 5 days as very low risk (Fig. 2). The most appropriate cutoff value to predict OHS occurrence was 30.0°C. Considering these facts, the current KMA heat index classification system has low utility as a heatstroke alert system. Unfortunately, the system is potentially dangerous because it invariably provides the public with a false sense of heat safety. Thus, all countries, including Korea, should implement an effective heat-safety alert system that reflects the characteristics of their specific location.
- There were several limitations to our study. First, we did not distinguish the difference between classic and exertional heatstroke; therefore, weather conditions might differently influence the types of heatstroke. Second, we had difficulties identifying the precise location of a heatstroke occurrence based only on a medical record review. Third, although climate conditions may be different locally within the same region at the same time, we could not consider this variability using the secondary data obtained from the KMA website. Therefore, it was impossible to accurately identify the real-life climate elements that affected the areas of OHS occurrence. Finally, as we did not use an individual level analysis such as case-crossover design, we could not adjust various covariates including patient’s age, sex, underlying health status, and so on.
- Nevertheless, to the best of our knowledge, this is the first Korean study to investigate the most relevant climate elements and their warning criteria to prevent heatstroke, with participation from all regional and local emergency medical centers. Furthermore, a large-scale medical review and regular quality control of the data were performed to ensure data accuracy and identify as many patients with suspected heatstroke as possible. Finally, we examined the correlations between heatstroke and climate elements using KMA’s climate data, identified the MHI as the most effective predictor of OHS incidence, and presented an appropriate cutoff value for the alert system.
- In the short term, it will be difficult to improve the environmental risk factors (including climate elements) that contribute to heat-related illnesses. However, the development and implementation of an effective alert system to inform the public of health risks and adequate response measures can provide a substantial preventive effect. Further systematic studies would be beneficial for the development of an effective heat alert system.
- We examined the correlations between climate elements and OHS in patients who were admitted to the local and regional emergency medical centers in Daegu. A total of 70 heatstroke patients were identified, 45 of whom experienced heatstroke outdoors. Although various climate elements were found to be correlated with heatstroke incidence, the MHI was closely associated with heatstroke incidence when all elements were considered simultaneously. The most predictive MHI cutoff point for OHS prevention was 30.0°C. Further studies are required to develop an effective heat alert system that incorporates the biometeorological characteristics of a specific location.
Discussion
| Variable | Outdoor (n=45) | Indoor (n=17) | Unidentified (n=8) | Total (n=70) | p-valuea) |
|---|---|---|---|---|---|
| Climate element | |||||
| Mean heat index (°C) | 32.6±4.6 | 33.7±2.4 | 34.5±1.4 | 33.1±4.0 | 0.228 |
| Mean air temperature (°C) | 29.4±2.9 | 30.4±1.8 | 30.8±0.9 | 29.8±2.5 | 0.106 |
| Maximal air temperature (°C) | 35.2±2.5 | 36.0±1.8 | 36.2±0.9 | 35.5±2.2 | 0.252 |
| Minimum air temperature (°C) | 24.3±3.3 | 25.5±2.1 | 25.8±1.4 | 24.7±3.0 | 0.100 |
| Daily temperature range (°C) | 11.0±1.9 | 10.5±1.5 | 10.3±1.9 | 10.8±1.8 | 0.394 |
| Mean relatively humidity (%) | 62.7±8.6 | 60.2±6.9 | 61.5±6.8 | 61.9±8.0 | 0.301 |
| Mean wind speed (m/sec) | 1.7±0.4 | 1.9±0.5 | 1.8±0.4 | 1.8±0.4 | 0.155 |
| Amount of sunshine (hr) | 9.7±2.4 | 10.0±3.5 | 9.5±2.6 | 9.8±2.7 | 0.722 |
| Heat index stage | 0.302 | ||||
| Very low | 7 (15.6) | 0 (0.0) | 0 (0.0) | 7 (10.0) | |
| Low | 9 (20.0) | 4 (23.5) | 0 (0.0) | 13 (18.6) | |
| Ordinary | 29 (64.4) | 13 (76.5) | 8 (100.0) | 50 (71.4) |
| Outdoor heatstroke day | Yes (n=34 days) | Noa) (n=508 days) | OR [95% CI] | aORb) [95% CI] |
|---|---|---|---|---|
| Mean heat index (°C) | 32.1±4.5 [22-39] | 26.0±4.2 [18-39] | 1.353 [1.217-1.504] | 1.708 [1.131-2.828] |
| Mean air temperature (°C) | 28.9±2.7 [22-32] | 25.0±2.9 [17-32] | 1.654 [1.375-1.988] | 0.776 [0.315-1.913] |
| Maximal air temperature (°C) | 34.8±2.4 [28-38] | 29.9±3.6 [19-37] | 1.713 [1.418-2.069] | 0.671 [0.265-1.669] |
| Minimum air temperature (°C) | 24.0±3.1 [16-27] | 21.3±2.9 [12-28] | 1.384 [1.182-1.622] | 1.492 [0.572-3.892] |
| Daily temperature range (°C) | 10.4±1.9 [7-15] | 8.2±2.8 [1-16] | 1.356 [1.166-1.578] | 1.770 [0.732-4.282] |
| Mean relatively humidity (%) | 60.7±8.8 [36-76] | 69.1±11.6 [32-97] | 0.941 [0.909-0.973] | 0.950 [0.879-1.027] |
| Mean wind speed (m/sec) | 1.2±0.5 [1-3] | 1.7±0.8 [0-5] | 0.392 [0.201-0.764] | 0.440 [0.180-1.078] |
| Amount of sunshine (hr) | 9.4±2.5 [2-12] | 5.1±4.0 [0-13] | 1.396 [1.212-1.608] | 1.220 [0.958-1.553] |
| Cutoff point for MHI (°C) | Sensitivity (%) | Specificity (%) | Youden’s index |
|---|---|---|---|
| 17.0 | 100.0 | 0.0 | 0.000 |
| 18.0 | 100.0 | 0.0 | 0.000 |
| 19.0 | 100.0 | 1.0 | 0.010 |
| 20.0 | 100.0 | 2.4 | 0.024 |
| 21.0 | 100.0 | 4.8 | 0.048 |
| 22.0 | 100.0 | 12.1 | 0.121 |
| 23.0 | 96.8 | 22.2 | 0.190 |
| 24.0 | 93.5 | 32.9 | 0.264 |
| 25.0 | 83.9 | 45.3 | 0.292 |
| 26.0 | 83.9 | 57.8 | 0.417 |
| 27.0 | 83.9 | 64.8 | 0.486 |
| 28.0 | 80.6 | 66.1 | 0.468 |
| 29.0 | 80.6 | 69.5 | 0.502 |
| 30.0a) | 77.4 | 73.7 | 0.511 |
| 31.0 | 61.3 | 79.6 | 0.409 |
| 32.0 | 61.3 | 88.1 | 0.494 |
| 33.0 | 58.1 | 92.7 | 0.507 |
| 34.0 | 41.9 | 97.2 | 0.392 |
| 35.0 | 35.5 | 98.6 | 0.341 |
| 36.0 | 19.4 | 99.4 | 0.188 |
| 37.0 | 12.9 | 99.8 | 0.127 |
| 38.0 | 3.2 | 99.8 | 0.030 |
| 39.0 | 3.2 | 99.8 | 0.030 |
- 1. NASA's Goddard Institute for Space Studies. July 2017 equaled record July 2016 [Internet]. Pasadena: Earth Science Communications Team at NASA's Jet Propulsion Laboratory; 2017 [cited 2018 Dec 20]. https://climate.nasa.gov/news/2618/july-2017-equaled-record-july-2016/.
- 2. Bouchama A, Knochel JP. Heat stroke. N Engl J Med 2002;346:1978–88.ArticlePubMed
- 3. Jardine DS. Heat illness and heat stroke. Pediatr Rev 2007;28:249–58.ArticlePubMed
- 4. Wang Y, Bobb JF, Papi B, Wang Y, Kosheleva A, Di Q, et al. Heat stroke admissions during heat waves in 1,916 US counties for the period from 1999 to 2010 and their effect modifiers. Environ Health 2016;15:83.ArticlePubMedPMCPDF
- 5. Yan YE, Zhao YQ, Wang H, Fan M. Pathophysiological factors underlying heatstroke. Med Hypotheses 2006;67:609–17.ArticlePubMed
- 6. Yaqub B, Al Deeb S. Heat strokes: aetiopathogenesis, neurological characteristics, treatment and outcome. J Neurol Sci 1998;156:144–51.ArticlePubMed
- 7. Kim DW, Chung JH, Lee JS, Lee JS. Characteristics of heat wave mortality in Korea. Atmosphere 2014;24:225–34.ArticlePDF
- 8. Kim J, Lee DG, Park IS, Choi BC, Kim JS. Influences of heat waves on daily mortality in South Korea. Atmosphere 2006;16:269–78.
- 9. Pryor RR, Bennett BL, O'Connor FG, Young JM, Asplund CA. Medical evaluation for exposure extremes: heat. Wilderness Environ Med 2015;26(4 Suppl):S69–75.ArticlePubMed
- 10. Kim SH, Jo SN, Myung HN, Jang JY. The effect of pre-existing medical conditions on heat stroke during hot weather in South Korea. Environ Res 2014;133:246–52.ArticlePubMed
- 11. Ghumman U, Horney J. Characterizing the impact of extreme heat on mortality, Karachi, Pakistan, June 2015. Prehosp Disaster Med 2016;31:263–6.ArticlePubMed
- 12. Alberini A, Gans W, Alhassan M. Individual and public-program adaptation: coping with heat waves in five cities in Canada. Int J Environ Res Public Health 2011;8:4679–701.ArticlePubMedPMC
- 13. Anderson GB, Bell ML, Peng RD. Methods to calculate the heat index as an exposure metric in environmental health research. Environ Health Perspect 2013;121:1111–9.ArticlePubMedPMC
- 14. Hajat S, Sheridan SC, Allen MJ, Pascal M, Laaidi K, Yagouti A, et al. Heat-health warning systems: a comparison of the predictive capacity of different approaches to identifying dangerously hot days. Am J Public Health 2010;100:1137–44.ArticlePubMedPMC
- 15. Kovats RS, Kristie LE. Heatwaves and public health in Europe. Eur J Public Health 2006;16:592–9.ArticlePubMedPDF
- 16. Toloo G, FitzGerald G, Aitken P, Verrall K, Tong S. Evaluating the effectiveness of heat warning systems: systematic review of epidemiological evidence. Int J Public Health 2013;58:667–81.ArticlePubMedPDF
- 17. Korea Meteorological Administration. [Korean climate resources] [Internet]. Seoul: Korea Meteorological Administration; 2019 [cited 2018 Dec 20]. http://www.kma.go.kr/weather/climate/average_south.jsp.
- 18. National Centers for Environmental Information. Climate change and variability [Internet]. Asheville: National Centers for Environmental Information; 2018 [cited 2018 Dec 20]. https://www.ncdc.noaa.gov/climate-information/climate-change-and-variability.
- 19. Sung TI, Wu PC, Lung SC, Lin CY, Chen MJ, Su HJ. Relationship between heat index and mortality of 6 major cities in Taiwan. Sci Total Environ 2013;442:275–81.ArticlePubMed
- 20. Jo YH, Shin SD, Kim DH, Jo IJ, Rhee JE, Suh GJ, et al. Descriptive study of prognostic factors of exertional heat stroke in military personnel. J Korean Soc Emerg Med 2003;14:409–14.
- 21. LoVecchio F. Heat emergencies. In: Tintinalli JE, Stapczynski JS, MA OJ, Cline DM, Meckler GD, Yealy DM, editors. Tintinalli’s emergency medicine: a comprehensive study guide. 8th ed. New York: McGraw-Hill Education; 2016. p. 1365–71.
- 22. Harlan SL, Ruddell DM. Climate change and health in cities: impacts of heat and air pollution and potential co-benefits from mitigation and adaptation. Curr Opin Environ Sustain 2011;3:126–34.Article
- 23. Marchetti E, Capone P, Freda D. Climate change impact on microclimate of work environment related to occupational health and productivity. Ann Ist Super Sanita 2016;52:338–42.PubMed
- 24. Murakami S, Miyatake N, Sakano N. Changes in air temperature and its relation to ambulance transports due to heat stroke in all 47 prefectures of Japan. J Prev Med Public Health 2012;45:309–15.ArticlePubMedPMCPDF
- 25. Schmeltz MT, Petkova EP, Gamble JL. Economic burden of hospitalizations for heat-related illnesses in the United States, 2001-2010. Int J Environ Res Public Health 2016;13:pii:E894.Article
- 26. Zhang Y, Nitschke M, Bi P. Risk factors for direct heat-related hospitalization during the 2009 Adelaide heatwave: a case crossover study. Sci Total Environ 2013;442:1–5.ArticlePubMed
- 27. Kravchenko J, Abernethy AP, Fawzy M, Lyerly HK. Minimization of heatwave morbidity and mortality. Am J Prev Med 2013;44:274–82.ArticlePubMed
- 28. Li Y, Li C, Luo S, He J, Cheng Y, Jin Y. Impacts of extremely high temperature and heatwave on heatstroke in Chongqing, China. Environ Sci Pollut Res Int 2017;24:8534–40.ArticlePubMedPDF
- 29. Williams S, Nitschke M, Weinstein P, Pisaniello DL, Parton KA, Bi P. The impact of summer temperatures and heatwaves on mortality and morbidity in Perth, Australia 1994-2008. Environ Int 2012;40:33–8.ArticlePubMed
- 30. Kenney WL, DeGroot DW, Alexander LM. Extremes of human heat tolerance: life at the precipice of thermoregulatory failure. J Therm Biol 2004;29:479–85.Article
- 31. Kosaka M, Yamane M, Ogai R, Kato T, Ohnishi N, Simon E. Human body temperature regulation in extremely stressful environment: epidemiology and pathophysiology of heat stroke. J Therm Biol 2004;29:495–501.Article
- 32. Canada. Health Canada. Health Environments and Consumer Safety. Heat alert and response systems to protect health: best practices guidebook. Ottawa-Ontario: Health Canada; 2012.
- 33. Josseran L, Fouillet A, Caillère N, Brun-Ney D, Ilef D, Brucker G, et al. Assessment of a syndromic surveillance system based on morbidity data: results from the Oscour network during a heat wave. PLoS One 2010;5:e11984.ArticlePubMedPMC
- 34. Li T, Ding F, Sun Q, Zhang Y, Kinney PL. Heat stroke internet searches can be a new heatwave health warning surveillance indicator. Sci Rep 2016;6:37294.ArticlePubMedPMCPDF
- 35. Méndez-Lázaro P, Muller-Karger FE, Otis D, McCarthy MJ, Rodríguez E. A heat vulnerability index to improve urban public health management in San Juan, Puerto Rico. Int J Biometeorol 2018;62:709–22.ArticlePubMedPDF
- 36. Nitschke M, Tucker GR, Hansen AL, Williams S, Zhang Y, Bi P. Impact of two recent extreme heat episodes on morbidity and mortality in Adelaide, South Australia: a case-series analysis. Environ Health 2011;10:42.ArticlePubMedPMCPDF
- 37. Sheridan SC, Kalkstein LS. Progress in heat watch–warning system technology. Bull Am Meteorol Soc 2004;85:1931–42.Article
- 38. O'Neill MS, Carter R, Kish JK, Gronlund CJ, White-Newsome JL, Manarolla X, et al. Preventing heat-related morbidity and mortality: new approaches in a changing climate. Maturitas 2009;64:98–103.ArticlePubMedPMC
- 39. Harlan SL, Chowell G, Yang S, Petitti DB, Morales Butler EJ, Ruddell BL, et al. Heat-related deaths in hot cities: estimates of human tolerance to high temperature thresholds. Int J Environ Res Public Health 2014;11:3304–26.ArticlePubMedPMC
- 40. Lee MS, Hong KJ, Shin SD, Song KJ, Ryoo HW, Song SW, et al. Development and implementation of emergency department based heat related illness active surveillance system: effect of heat index on daily emergency department visits due to heat related illness. J Korean Soc Emerg Med 2014;25:595–601.
- 41. Bai L, Ding G, Gu S, Bi P, Su B, Qin D, et al. The effects of summer temperature and heat waves on heat-related illness in a coastal city of China, 2011-2013. Environ Res 2014;132:212–9.ArticlePubMed
- 42. Kalkstein AJ, Sheridan SC. The social impacts of the heat-health watch/warning system in Phoenix, Arizona: assessing the perceived risk and response of the public. Int J Biometeorol 2007;52:43–55.ArticlePubMedPDF
References
Figure & Data
References
Citations

- Ambient heat exposure and kidney function in patients with chronic kidney disease: a post-hoc analysis of the DAPA-CKD trial
Zhiyan Zhang, Hiddo J L Heerspink, Glenn M Chertow, Ricardo Correa-Rotter, Antonio Gasparrini, Niels Jongs, Anna Maria Langkilde, John J V McMurray, Malcolm N Mistry, Peter Rossing, Robert D Toto, Priya Vart, Dorothea Nitsch, David C Wheeler, Ben Caplin
The Lancet Planetary Health.2024; 8(4): e225. CrossRef

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine
 PubReader
PubReader ePub Link
ePub Link Cite
Cite